MercyOne is the largest health system in the State of Iowa, with a staff of over 20,000 professionals across 100 clinics and seven hospitals around the State. “We treat the entire care continuum, from urgent care to emergency departments, hospital stays and tertiary care,” says Stephen Nielson, Manager of Digital Health at MercyOne.
There was a time when people would wonder what you meant by “digital health”. Beyond typing up people’s health records to a computer, you would have been hard-pressed to find applications for digital technology in the health sector. But over the last 20 years in general, and the last five years in particular, attitudes have changed significantly.
“I first came into the health system as a student in the early 2010s, when EHRs (electronic health records) were big news,” Nielson recalls. “The government had just mandated the use of electronic health records and organisations were trying to adapt. Along with those records came the promise that your patient portal would modernise healthcare and give patients access to their information.”
EHRs have already done a lot of good in the healthcare sector, but the adoption of digital and virtual products has been slow despite ever-increasing expectations that these tools would be available. Then, of course, we all had to reassess the role of digital tools in the workplace.
“Since I launched my career, the pandemic changed everything,” Nielson shares with us. “It brought online scheduling and virtual visits to the forefront for everyone. It forced our organisation to rethink our approach to these tools and how we want to present them to patients. Patients, meanwhile, have come to expect this as an option for them. We saw that we needed to maintain a continuity of care with patients across multiple settings, not just treating people who are sick but managing their care on a day-to-day, month-to-month basis.”
 Hospital Level Care in the Home
Hospital Level Care in the Home
One word in particular that we have started to hear across the healthcare sector is “telehealth”. It is transforming the way patients interact with their medical practitioners.
“What I was taught by my mentors is that having digital and virtual departments in a health system is not its own strategy,” Nielson tells us. “Our job is to equip and empower patients, providers and our colleagues within the organisation. Our mission is to improve on our weaknesses. Telehealth does not mean giving healthcare providers a camera and a Zoom account and expecting them to increase the utilisation of telehealth or advertise it to patients. We need to start with what the providers need and clarify what we are trying to accomplish and how telehealth can be used as a tool to do that.”
Nielson points to the difficult weather that is common in the Mid-West. It is not uncommon for travel to be made difficult by circumstances such as blizzards, but telehealth solutions are a way to work around that.
“An area that is really exciting for me is that we are working on virtual nursing,” Nielson shares. “We are going through our hospitals and implementing TVs and cameras and microphones in a lot of our hospital rooms. Then we have a team of nurses in a centralised hub who can provide support to the on-site nurses. If a patient is uncomfortable, a nurse can just come up on the TV and check in on the patient, keeping them calm until they have help. They can also provide more junior nurses with training and oversight.”
It is a particularly useful tool when so many nurse graduates are still learning on the job and can benefit from remotely offered support and advice.
At the same time, remote patient monitoring is becoming an increasingly valuable tool across the whole healthcare sector, where in-patient care is no longer seen as the pinnacle.
“We are focusing on patients who have been discharged from the hospital with sepsis. We can send them home with a blood pressure cuff, a heart rate monitor and thermometer to track their vitals, similar to the way a virtual nurse would,” Nielson says. “We have nurses to monitor those daily readings and make sure those patients stay healthy, or sound the alarm if they do not.”
Finally, Nielson is also keeping a close eye on whether artificial intelligence could have applications in the sector, but with a due sense of caution.
“We are finding out what’s safe and useful, while making sure we keep patient data secure and avoiding hallucinations in the technology,” says Nielson says.
 Meeting the Patient Where They Are
Meeting the Patient Where They Are
Nielson is similarly pragmatic around the application of telehealth technology.
“Telehealth is a tool, not a strategy in itself,” he emphasises.
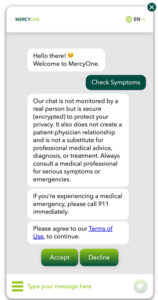
To realise the potential of these tools, it is essential that MercyOne ensures its patients are comfortable with the technology.
“Usability is one of the biggest issues,” Nielson says. “The question we are always asking is ‘How do you make a good idea simple enough for everyone?’ How can it be accessible and intuitively make sense? As a digital native, it is all you have ever known, but some patients might be daunted by having to make sure their camera and microphone are working correctly.”
But as well as making sure that the technology is usable, it is also important to check that the technology actually improves the quality of care in practice.
“If you implement technology without proper input from care staff, you will later discover the unforeseen reasons why it made their jobs more difficult,” Nielson warns. “That’s where we have had to take a step back and get input upfront from all parties. This is how working in healthcare IT is unique. We have two customer bases, patients and healthcare providers.”
When it comes to meeting the needs of patients, their healthcare needs and their level of comfort with technology must both be dealt with alongside the issue of payment.
“The American healthcare system has a disparate payment system, with multiple kinds of insurance that need to be factored in and understood,” Nielson says. “There is a lot of disconnect between different sites of care for patients, and we need to understand that healthcare is costly and difficult for many patients. Patients consider cost as a key part of access to care in the States. That is a barrier. We aim to be more efficient, avoiding instances of unnecessary care to bring down costs. We want to focus on how we can meet patients where they are at. We have a reputation within our communities of being a great place to get care and a great place to work, where patients are going to be healed.”
It is a reputation that Nielson seeks to build on in how he applies technology to healthcare at MercyOne going forward.







